Placenta Accreta
Placenta Accreta Definition
Placenta accreta happens when all of the placenta or a part of it is abnormally attached to the myometrium. Based on the normally anatomy of the placenta, it is always attached to the wall of the uterus; but in placenta accreta, its blood vessels and other parts are growing too deeply into the wall of the uterus.
After delivery of the baby, the placenta is expected to be completely detached from the uterine wall and be delivered during placental separation in the fourth stage of labor and delivery process. The patient who has placenta accreta will have a part of her placenta, still firmly attached with uterine wall, and this can pose a great risk for possible bleeding.
Placenta accreta is a life-threatening complication of the pregnancy. The incidence of its occurrence accounts for approximately 75% of the cases with placental problems, placenta increta 15% of all cases and placenta percreta is 5% among all cases.
Symptoms of Placenta Accreta
Patients with placenta accreta are often asymptomatic at the time of the pregnancy, though there are instances that vaginal bleeding may happen during the third trimester.
Clinical symptoms are seen when the woman delivers the baby, as followed by placental delivery where any member of the health team can assess and evaluate the status of the placenta in relation to its attachment with the uterine wall.
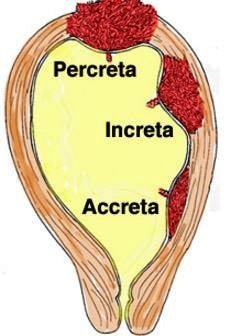
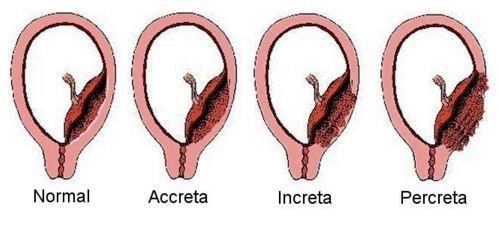
There are three variants of placenta accreta:
- Accreta is when the placenta is attached to the muscles of the wall of the uterus
- Increta is when the placenta extends itself into the uterine muscles
- Percreta is when the placenta is extended throughout the entire uterine wall
Risk factors
There are several factors which might increase the woman’s risk to develop placenta accreta and these are:
- History of previous uterine surgery such as cases of cesarean birth or other surgical procedures of the uterus
- Position of the placenta such as in placenta previa, where the placenta is partially or completely covering the cervix
- History of previous pregnancy so that the woman is more prone to have the problem during each period of the delivery
- Conditions of the uterus such as when the placenta gets implanted over a uterine scar, and noncancerous growths of the uterus that is bulging into the uterine cavity
- Uterine lining that is scraped during dilatation and curettage
Pathogenesis
The exact cause of placenta accreta is not known yet. Some studies have shown that this pregnancy complication is linked with a woman’s history of placenta previa or experiences of previous cesarean birth. This problem accounts a range of about 5% to 10% of reported cases who have placenta previa.
It has also been noted that the more the woman underwent through cesarean delivery, the more chances she will have to be at risk for future chances to have placenta accreta. It takes about an approximate of 60% of patients with placenta accreta also have multiple cesarean births.
Diagnosis
An attending physician may recommend examinations to support confirm the diagnosis of placenta accreta in the presence of potential risk factors with a pregnant woman to develop such problem.
Imaging tests used to evaluate the implantation of the placenta in relation to the uterine wall:
- Ultrasound
- Magnetic resonance imaging
Sonographic findings that can suggest an existing placenta accreta:
- Normal hypoechoic retroplacental zone is lost
- Presence of irregular vascular spaces within the placenta
- Bridging or linkage is noted from the blood vessels or placental tissues in relation with the uterine serosa, myometrial bladder interface or with the uterine placental margin
- Measurement of retroplacental myometrial thickness is lesser than 1mm
- Visualization of numerous coherent vessels
Maternal alpha-fetoprotein is a blood test to assess the protein level produced by the baby, since an elevation is associated with placenta accreta.
Treatment
The attending physician usually plans with the patient and the family to safely deliver the baby in the suspicion of placenta accreta.
Cesarean hysterectomy is the delivery of the baby by way of Cesarean route, followed by a hysterectomy in order to surgically remove a problematic uterus. This helps to prevent massive blood loss which can possibly occur as the placenta remains firmly attached to the uterine wall.
When a patient has plans for another future pregnancy, a thorough discussion has to be done to keep the uterus intact instead following the cesarean birth, but it has to depend on the severity of the problem with the placenta.
Post-operative management:
- Pitocin
- Antibiotics
Conservative management techniques to spare uterine removal:
- Leaving the placenta intact in the uterus
- Curettage of the uterus
- Application of an intrauterine balloon catheterization
- Embolization of the pelvic vessels
- Ligation of the internal iliac artery
- Ligation of the bilateral uterine artery
Complications
Placenta accreta can end up with the following life-threatening complications:
- Premature delivery of the baby since there might be a need for early delivery of the baby as the labor process may be initiated earlier than expected.
- Massive vaginal bleeding of the woman may result after the delivery of the baby as al or a portion of the placenta might not be delivered successfully due to a problem on attachment with the uterine wall. The hemorrhagic bleeding prevents the normal clotting to occur, and might result with an adult respiratory distress syndrome. Patients may need a blood transfusion.
References:
- Placenta Accreta: Symptoms, Risks And Treatment, What is the difference between accreta, increta or percreta?, What are the risks of placenta accreta to the baby & Mother? http://americanpregnancy.org/pregnancy-complications/placenta-accreta/
- http://www.healthline.com/health/pregnancy/preterm-labor-delivery-placenta-accreta
- Placenta Accreta: Causes, Risk factors, Complications, Preparing for your appointment, Tests and diagnosis, Treatments and drugs, Coping and support http://www.mayoclinic.org/diseases-conditions/placenta-accreta/basics/symptoms/con-20035437
- Johnston, T A; Paterson-Brown, S (January 2011). Placenta Previa, Placenta Previa Accreta and Vasa Previa: Diagnosis and Management. Green-top Guideline No. 27. Royal College of Obstetricians and Gynecologists.
- Arulkumaran, edited by Richard Warren, Sabaratnam (2009). Best practice in labour and delivery (1st ed., 3rd printing. ed.). Cambridge: Cambridge University Press. pp. 108, 146.
- Turrentine, John E. (2008). Clinical protocols in obstetrics and gynecology (3rd ed.). London: Informa Healthcare. p. 286.
